Animal Experiments Lead Science Astray, Leaving Human Patients Suffering
Psychedelic drug therapies may hold the key to effective treatment of a variety of mental health disorders, including post-traumatic stress disorder (PTSD), major depression, anxiety, eating disorders, and addiction.
But effective psychedelic drug development for these disorders risks getting bogged down by the same ineffective and cruel system of animal experimentation that has stymied the creation of other psychiatric drugs.

The therapeutic potential of psychedelics is facing scrutiny due to problem-ridden clinical trials and poor reproducibility in preclinical studies. Psychedelic research needs a paradigm shift, moving beyond the outdated animal models used in the 1960s, otherwise the field once again risks losing support.
Futile Animal Experimentation
The problem is easy enough to understand. Other animals simply are not miniature humans. The significant physical, biological, genetic, and physiological differences between species render the results of experiments on animals questionable at best.
Experimenters often assume that observed animal behaviors accurately reflect complex human psychiatric conditions. It’s a ‘leap of faith’ disguised as scientific inquiry and part of the reason treatments for mood and anxiety disorders are no more effective than they were 50 years ago.

For example, the widely discredited forced swim test has for years been used as a model for human depression. It is not. And even the National Institute of Mental Health now discourages experimenters from using it, being recently joined by the National Health and Medical Research Council in Australia, which won’t fund it anymore. The Australian state of New South Wales has even made it illegal and the U.K. might do so soon as well.
Psychedelic research uses this and other similar bunk tests. Enter the head twitch response test.
A mouse or a rat sometimes will rapidly and rhythmically twitch its head after psychedelic drugs have reached a specific portion of the brain. Some experimenters claim the test can predict whether a compound will reach humans’ brains, despite the prevalence of false positive results to different compounds. The test does not correlate with any meaningful symptom seen in human psychiatric disorders nor human psychedelic use.
Humans do not twitch their heads after taking psychedelics. Watching a mouse shake their head doesn’t provide any insight into symptoms of human psychiatric diseases and is not a necessary or reliable way to test drug delivery.
Like the forced swim test, the head twitch test is also cruel. Experimenters cut into an animal’s scalp and cement a magnet on their skull or pierce their ears with a magnet without pain relief.
Led Astray
In clinical psychiatry, psychiatrists often rely on previous experience and observation to monitor a patient’s reaction to a particular drug. Exactly how many antidepressants work in humans simply isn’t understood, despite that these drugs are among the most prescribed psychiatric medications.
As an example, the foundational theory for the existence of human depression is called the serotonin hypothesis, which says reduced levels of brain serotonin cause depression. It’s taught to doctors-in-training and often used to explain the cause of depression to patients.

But this theory, which was based on experiments on animals, has begun to be questioned. A 2023 systematic review found no consistent evidence linking serotonin to depression in humans. There’s an urgent need to reassess drug development practices, including the continued reliance on animal models in psychiatric research.
Sound Science Begets Sound Science
Animal experimentation need not continue. Alternatives exist, such as various in vitro techniques, ranging from traditional 2D cell cultures to 3D tissues. The technology known as organs-on-chips has been used to assess drug delivery to the brain for psychiatric and neurological conditions such as Alzheimer’s disease.
Noninvasive, human biology-based models allow researchers to replicate studies more readily and verify previous conclusions—a hallmark of good science that is often not possible with experiments on animals. They also serve as a consistent benchmark that enables scientists to accurately compare newly developed drugs and ensure future studies build on standardized, validated methods.

Troding the same well-worn animal experimentation path will continue to hinder medical progress. Tormenting and killing animals for the sake of consistency perpetuates this flawed cycle and hampers meaningful research.
Diverting funding toward models that use human cells and data to evaluate the delivery and efficacy of psychedelic drugs is essential for science and for the patients who need and deserve effective treatments.
What You Can Do
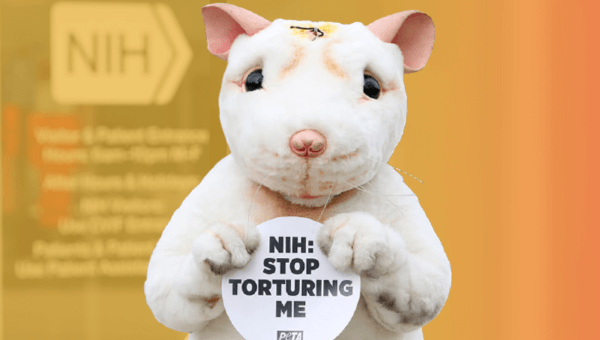
It’s time for the National Institutes of Health to advance science and align with Americans’ growing commitment to animal welfare by ending cruel animal experiments.
U.S. residents can take action by urging members of Congress to mandate that the National Institutes of Health stop throwing away taxpayer money on useless animal experiments and instead invest in modern, non-animal research methods.
And everyone can take action by urging the National Institutes of Health to stop funding pointless and deadly sepsis experiments on animals.